If it suddenly feels like a lot of people you know have been infected with COVID-19 this summer, you’re not alone.
COVID-19 is on the rise again in the Chicago area and across the nation, marking the fourth consecutive summer the country has seen an increase in cases.
“It’s not going away,” said Dr. Robert Murphy, director of the Havey Institute for Global Health and professor of infectious disease medicine at Northwestern University Feinberg School of Medicine. “We’ve personally seen a significant increase in the number of cases and the number of prescriptions being written for paxlobidi, the treatment that’s currently available.”
According to the Chicago Department of Public Health, the positive COVID-19 test rate in Chicago for the week ending July 13 rose to 9.8%, up from 2.5% for the week ending June 1. The department also found that over the past three weeks, eight of Chicago’s 11 monitored wastewater treatment plants have seen elevated concentrations of the COVID-19 virus in their wastewater.
Nationwide, concentrations of the COVID-19 virus in wastewater are high, with a test positivity rate of 12.6% for the week ending July 13, according to the Centers for Disease Control and Prevention. On the West Coast, the test positivity rate for the same week was 16.4%.
Local health systems are also noticing the increase: Laboratories at Edward and Elmhurst hospitals saw 256 positive COVID-19 tests in the week ending July 20, up from 66 in early June, according to Dr. Jonathan Pinsky, medical director of infection control at Endeavor Health Edward Hospital in Naperville.
Pinkey said he’s “not particularly surprised” by the recent surge in cases, given similar cases this past summer, and doctors say it’s likely many sick people aren’t even being tested.
It’s not entirely clear why COVID-19 cases continue to rise during the summer, when rates of the respiratory disease are lower, but doctors say waning immunity from the vaccines many people received in the fall could be related to the virus’s continued mutations. FLiRT variants According to the CDC, the majority of cases nationwide are currently due to influenza.
“Influenza viruses do not do well in the summer, they are less survivable and less transmissible,” Pinsky said. “I think this virus is different. It’s definitely more transmissible in the winter, but there’s something about the virus that makes it transmissible in the summer.”
The good news is that the increase in cases this summer has been nowhere near the magnitude of the big spikes earlier in the pandemic. This winter’s COVID-19 wave.
“We may be seeing a slight increase in patient volume, but nothing noteworthy,” said Dr. Michael Cui, a primary care physician at Rush Primary Virtual First in Chicago. He said he’s seen a 10 to 15 percent increase in paxlobidi prescriptions in recent days. “It’s not a massive increase, going from one or two patients one day to 30 the next… We’re not seeing a flood of patients, though.”
There’s more good news: Although hospitalizations nationwide have been gradually increasing in recent weeks, they remain relatively low, as have COVID-19 deaths, likely in part because doctors say nearly everyone now has some immunity to the disease, having already been infected, vaccinated, or both.
“The severity of infections has decreased significantly,” Pinsky said. “Patients with infections severe enough to require oxygen or intensive care are uncommon and are significantly less common than they were two years ago.”
But people with weakened immune systems or certain underlying health conditions remain at risk for more severe illness and may want to continue taking precautions like wearing masks and avoiding crowds, Murphy said.
Pinkey said common symptoms of COVID-19 include a stuffy nose, sore throat and cough, and some people may also experience headaches and fevers. And while severe symptoms are less common, Murphy said people who previously had mild symptoms can now become very ill with COVID-19.
“Just because it’s been calm in the past doesn’t mean it’s going to be calm this time,” Murphy said.
The CDC’s latest guidelines for people infected with any respiratory virus, including COVID-19, are to stay home and avoid contact with others until they have been fever-free for 24 hours without the use of fever-reducing medication and their overall symptoms have improved within 24 hours. After that, the CDC recommends taking other precautions to prevent the spread of the disease, such as wearing a mask for five days after returning to normal activities.
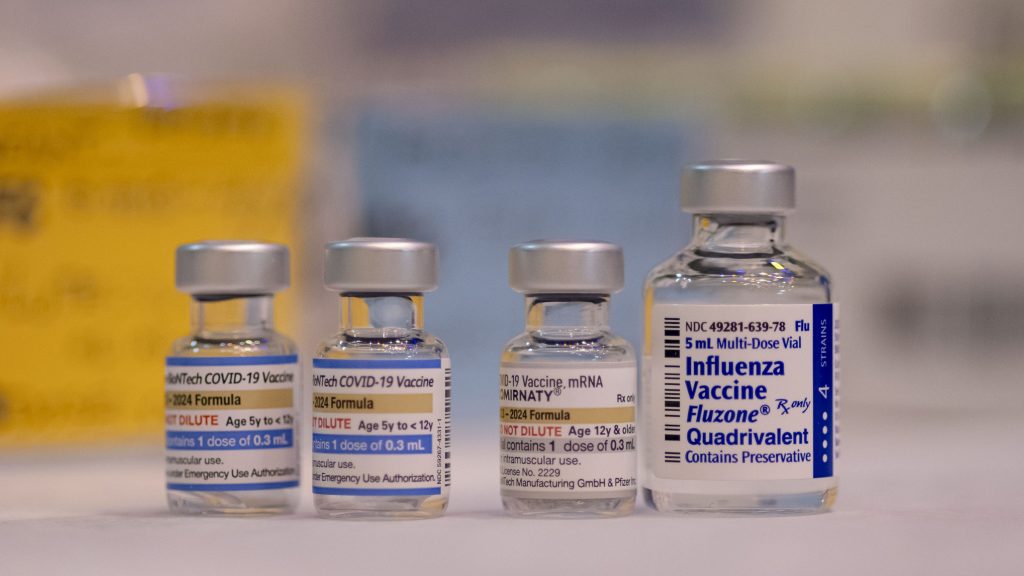
Antiviral medications such as Paxlobidi can be used to treat COVID-19. Paxlobidi is recommended for people at high risk of severe illness.
Doctors also recommend keeping your COVID-19 vaccine up to date to reduce the risk of severe illness. According to the Chicago Department of Public Health, about 16.5% of people across Chicago had kept their COVID-19 vaccine up to date as of July 20.
“There are things you can do to help yourself,” Murphy said.
First published: