One of the best-known neuropathic pain relieving phenomena, the placebo effect, has not been fully understood for centuries. In an important development, researchers at the University of North Carolina at Chapel Hill have now tricked a group of mice into expecting pain relief when in fact it wasn’t, and in the process identified specific brain circuits that appear to play a key role in this process.
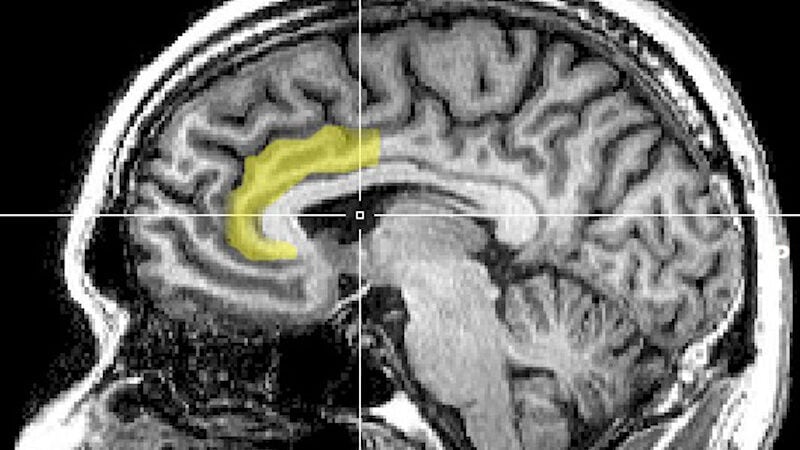
The effect of administering substances that have no actual medicinal effect on patients, resulting in improvement in their condition, has been well documented dating back to the 18th century. 18th centuryPrevious experiments have established that activity in specific parts of the brain correlates with the placebo effect, but the exact mechanism of how it works remains a bit of a mystery. Indeed, when patients respond to placebos to relieve pain, brain images show activity in the anterior cingulate cortex (an area involved in processing pain), but explanations for this remain somewhat hazy. Now, scientists at UNCCH think they have narrowed down how this works.
their studyPublished in this week’s journal NatureThe scientists trained mice by placing them in two connected chambers for a week. For the first few days, the floors in both chambers were comfortably warm. Then, the floor in one chamber became painfully hot, but the mice were able to escape the pain by running around. On the final day, the floors in both rooms were painfully hot. The mice, who had been conditioned to expect pain relief when they reached the second room, experienced some pain relief due to the placebo effect. When they reached the second room, even though it was just as hot as the first, The mice showed less injury-related behavior, such as hopping or licking their paws.
Importantly, mice were injected with a modified virus that allowed the researchers to monitor specific neurons in a region of the brain called the anterior cingulate cortex.The mice were connected to three other regions, including the pontine nucleus, which is crucial for mastering motor skills and had not previously been found to be involved in processing pain, but when the mice ran into chamber 2, neurons connecting the two regions lit up.
When the researchers artificially activated this neural pathway in a new group of susceptibility-tested mice, the mice exhibited less re-injury behavior, suggesting that this neural circuit plays an important role in placebo-induced pain relief.
In the study, the authors acknowledge that pain is complex and that the placebo effect in humans may be more complicated than that seen in mice, but they expressed hope that their research may lead to new drugs or behavioral therapies that relieve pain.