COVID-19 is on the rise again, with virus levels “very high” across the country, including in Washington, D.C., and Maryland. According to data from the Centers for Disease Control and Prevention.
America saw an upswing in COVID-19 cases last summer as well, but a lot has changed since then. Ever-evolving variants, directives from health officials, and the behavior of the people around us can be confusing, to say the least.
So how do we navigate this latest outbreak? Should I be worried about COVID-19 anymore? Are the symptoms of the latest variant any different? Should I still test myself? Are rapid tests trustworthy? Do I need to stay home if I have the virus?
News4 spoke with several health and infectious disease experts to get answers to these questions and more.
Please check this guide for ongoing updates as new information becomes available.
Is COVID still a thing? Isn’t it just like having a cold at this point?
“COVID-19 is still important, it’s just not as important as it was two years ago or three years ago, but it’s definitely important because we’re always concerned about getting sick, and getting sick is never a good thing,” said Dr. Emily Smith, an associate professor at the George Washington University Milken Institute School of Public Health.
For most people, COVID-19 has become just another respiratory virus they have to deal with, said Dr. Amesh Adalja, an infectious disease expert and senior scholar at the Johns Hopkins Center for Health Security, but at the same time, the virus is still causing hospitalizations and deaths.
“If you’ve just had a lung transplant, then of course you should be concerned. But if you’re a healthy 18-year-old, it may not be as important. COVID-19 affects everyone differently. No two cases are the same,” he said.
Adalja said it makes sense that with each new case count, the virus will have less of an impact on people’s lives.
“With endemic respiratory viruses, it becomes part of the human condition. Any time you come into contact with other humans you’re at risk, but because we have tools — vaccines, home testing, antivirals, wastewater monitoring — we have more tools than other respiratory viruses, so it’s much more manageable for the majority of the population,” Adalja said.
Dr. Prajna Patel, chief medical officer for the U.S. Department of Health and Human Services/Centers for Disease Control and Prevention, told News 4 it’s important people remain vigilant as more information continues to emerge about the long-term health effects of COVID-19.
Newly released CDC data A study from 2022 found that more than 10% of adults with disabilities experienced long-term symptoms of COVID-19, and those symptoms were more common among adults with disabilities than among adults without disabilities.
Why are we seeing another surge in COVID-19 cases in the summer?
Medical experts say a combination of three factors created the perfect storm for this summer’s coronavirus outbreak: new variants that evade the immune system, a population with weakened immune systems and extreme heat that forced more people indoors.
Just as respiratory viruses spread in the winter when many people gather indoors for holidays and to stay warm, COVID-19 also tends to ripple through the summer when people gather indoors to escape the heat.
“It’s so hot, we’re staying inside, traveling and attending summer weddings,” Smith said.
“Three years ago, two years ago, we thought this summer wave would be over, but it’s back. This virus is very good at infecting people who are indoors, so I think the extreme heat and summer fun is at least partially responsible for the waves we’re seeing now,” Smith said.
What are the COVID-19 infection rates and hospitalizations like?
D.C. and Maryland are among 22 states nationwide that ‘Very high’ COVID-19 wastewater virus activity levelsand the latest statistics show that as of July 16, 42 states and territories are experiencing increases or possible increases in COVID infections. CDC data.
Nationwide, levels of COVID virus activity in wastewater are “high,” according to the CDC. Virginia’s COVID activity is also in the “high” range.
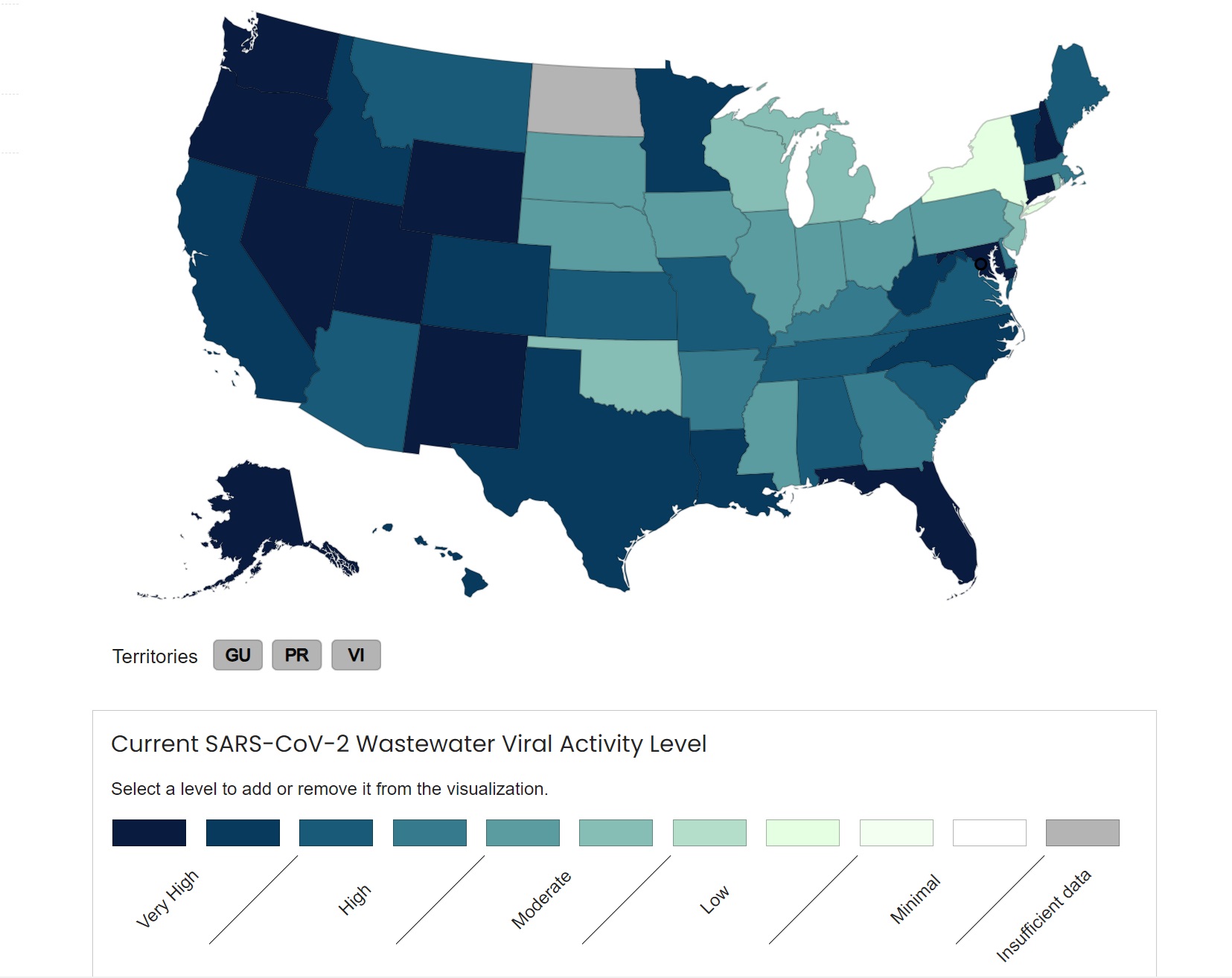
Although virus activity levels have increased over the past month, wastewater testing in the Northeast has found that virus activity levels remain much lower than in January.
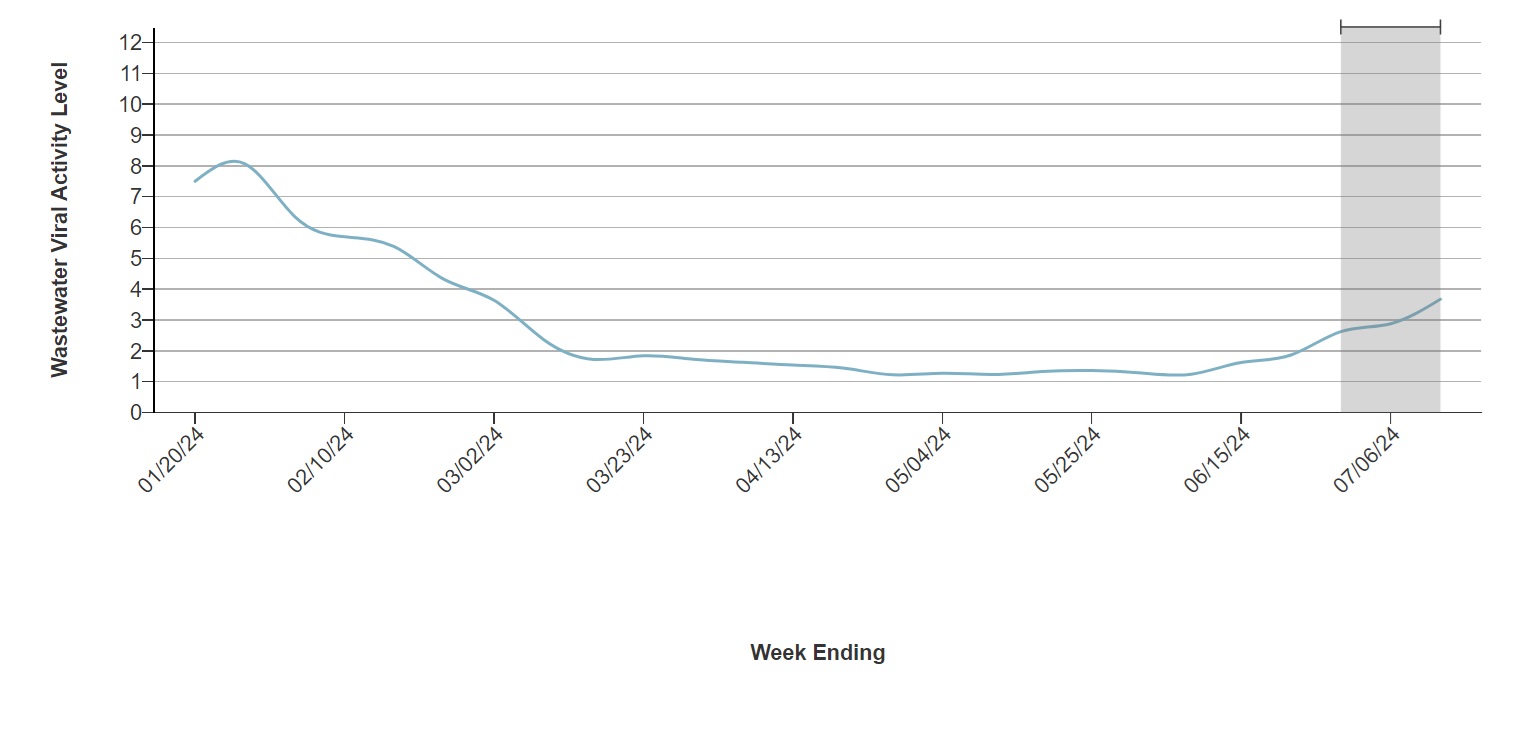
Patel said sewage samples indicate the spread of the virus but don’t necessarily correlate with an increase in hospitalizations.
“We are not seeing an increase in hospitalizations or deaths in this latest surge in cases, which is very reassuring,” she said.
Emergency departments in Maryland and Virginia have seen an increase in COVID patients in recent weeks. Data Show.
“The primary metric we are monitoring COVID-19 activity is emergency department visits. Currently, approximately 3.3% of all emergency department visits are being diagnosed with COVID-19. This is up from 1.2% from the beginning of the summer through early June,” Mandy Barton with the Fairfax County Health Department told News 4 on July 18.
What COVID variant is currently predominant?
The variant, called KP.3, is part of a family of variants that scientists have dubbed “FLiRT” and is steadily spreading The number of cases in the United States has increased in recent weeks..
As of July 20, KP.3 is estimated to account for 33% of cases. According to the CDC:Another variant, KP.3.1.1, has quickly become the most dominant variant, accounting for approximately 18% of cases.
Do FLiRT variants cause different symptoms?
“The symptoms caused by infection with the FLiRT variant are largely indistinguishable from other versions of the virus,” Adalja said. “Symptoms are varied and will vary from person to person, but in general, any upper respiratory symptoms such as cough, sore throat, runny nose, muscle aches, pain, and fever may be part of the common symptom cluster of COVID-19.”
Just to let you know, the typical symptoms are:
- sore throat
- cough
- Malaise
- congestion
- snot
- headache
- muscle pain
- Fever or chills
- New loss of taste or smell
- Shortness of breath or difficulty breathing
- Nausea or vomiting
- diarrhea
What are the CDC’s current quarantine guidelines?
of CDC updates quarantine guidelines The government announced earlier this year that it was no longer recommending that people self-isolate at home for five days if they test positive for COVID-19, regardless of symptoms.
Instead, the CDC says that if you have symptoms or test positive for the virus, you should stay home and avoid contact with others, but you can resume normal activities once you’ve been fever-free for 24 hours without the help of fever-reducing medication.
“Basically, they’re saying if you’ve been fever-free for 24 hours and your symptoms are improving, you can stop isolating,” Patel said. “I would say you should be cautious for five days after you stop isolating, which means if you go back to work and have meetings with colleagues, it may be important to sit apart, wear a mask, etc. because we know that you can continue to shed virus and be infectious even after your fever has subsided.”
other CDC Recommendations include:
- Take steps to improve ventilation in your home
- Reinforce hygiene habits and wash your hands frequently
- If you must be around others at home or in public, wear a well-fitting mask.
- Keep your distance from others
- Virus testing continues
Can rapid tests detect the latest COVID variants?
Yes, infectious disease experts agree that rapid tests are still a reliable way to test for COVID, even as new variants emerge.
“Rapid tests work for any of these variants because what they’re looking for is a part of the virus that hasn’t mutated as much,” Adalja said. “When we talk about variants, we’re talking about mutations that are happening in the spike protein. Antigen tests don’t look for the spike protein, they look for another part of the virus.”
That being said, Adalja explained that timing and frequency play an important role in getting accurate results from at-home tests.
“[The rapid test] “When you first start to have symptoms, the rapid test may be negative because the symptoms are caused by your immune system and not the virus. The virus has to reach a certain level for the rapid test to be positive,” he said. “If you have symptoms and the rapid test is negative, you may want to test again in a few days, or get a PCR test, or it could be a completely different virus and you’ll need to be tested for a different type of virus, or it could be a bacterial infection like strep throat.”
What are the guidelines on when to get a rapid test?
According to Covid.gov, you should get tested at home if:
- You start to experience COVID symptoms, such as fever, sore throat, runny nose, and loss of taste or smell.
- At least 5 days after close contact with a person with COVID-19
- Before gathering in groups, especially if the group includes people who are at risk for severe illness or who may not be up to date on vaccinations.
Many tests have extended expiration dates. Click here for details About approved at-home diagnostic tests and their expiration dates.
Will my insurance cover the cost of a rapid at-home COVID test?
Most insurance plans are required to cover the cost of up to eight at-home tests without a prescription every 30 days. According to CVS:.
National pharmacy chains such as Walgreens and CVS are allowing customers to submit claims online and check whether their insurance company covers the rapid tests.
Are there any new COVID vaccines in the works?
A new vaccine is expected to arrive this fall. In the meantime, the COVID-19 vaccines released last year will likely still offer some protection, Patel said.
If someone tests positive for COVID-19, what treatments should they consider?
While you’re recovering, be sure to rest, drink plenty of fluids, and monitor your symptoms.
Older adults and others at high risk for severe illness from COVID-19 should talk to their doctors about treatments for the virus that may reduce the chance of hospitalization or death, the CDC recommends.
“So even if symptoms are mild, people who are symptomatic may be candidates for treatment, for example, people over 65, people who may be immunocompromised, people of any age who have chronic conditions such as heart disease, lung disease, obesity, diabetes or chronic kidney disease,” Patel said. “And these people should not delay in contacting their health care provider who may want to start testing and treatment as soon as possible so they don’t have to go to the hospital.”
Antiviral drugs such as paxilovir and remdesivir work to stop the virus from spreading and multiplying in the body. For more information on antiviral treatments, click here.
What can you do to prevent COVID-19 infection?
Ways to prevent catching or spreading COVID-19 include getting vaccinated, practicing good hand hygiene, wearing a mask in crowded places, gathering outdoors and improving ventilation by opening windows or using portable filters.
“If you are someone who is at high risk for complications from COVID-19 and you are in a crowded congregate setting, you may want to be aware that the virus is likely to be present in that room and consider wearing a mask appropriately in those situations,” Adalja said.